Cost of an Ultrasound System

Understanding the Cost of Owning an Ultrasound SystemPoint-of-care ultrasound (POCUS) has become an essential tool in modern medicine, but how much does owning one really cost? When considering POCUS for your practice, understanding the full picture of costs involved—from initial purchase to system maintenance—is crucial. …
#PracticeMakesPOCUS
Clinicians often struggle with the complexities of mastering POCUS scanning techniques. It's not the tech they struggle with, it's the scanning. Discover Sonosite Scan Along - available on all our newest FUJIFILM Sonosite systems. …
Did You Know that Sonosite has a New Vascular Access Education Partner?
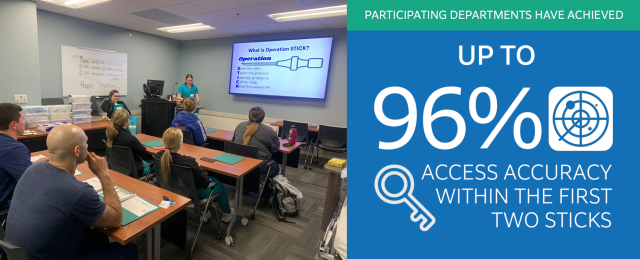
Did You Know that FUJIFILM Sonosite has a new partner to provide vascular access education to our customers? With education being one of our core pillars, we strive to ensure that your department and clinicians are adequately equipped with the knowledge and training to administer care to patients using point-of-care ultrasound. …
Better Patient Outcomes through POCUS Practice and Clinical Training

Training MattersPoint-of-Care Ultrasound (POCUS) empowers clinicians with real-time diagnostic capabilities and procedural practices at the patient's bedside, which can improve the speed and accuracy of patient care. Hands-on POCUS training for clinicians at educational workshops is imperative in maximizing the benefits of using ultrasound systems effectively. …
Designed for Durability: The Rigorous Testing Process of Sonosite Transducers
Introduction: Setting the Bar HighIn Point-of-Care-Ultrasound, the durability of equipment is paramount. Without quality systems that are ready to use, the immediacy of patient care can be negatively impacted. To ensure reliability and up-time, Sonosite transducers are tested to the limit. This process consists of extensive testing protocols that go beyond industry norms. …
Empowering Healthcare Providers with Sonosite's Voice Assist

In today's healthcare landscape, institutions face a daunting challenge: maintaining high-quality patient care, often with limited staffing.
…
Joining the Mission with the Friends of Fiji Heart Foundation

The Mission
Since the formation of the Friends of Fiji Heart Foundation (FOFHF) in 2006, the Foundation has sent a mission to Fiji for each successive year to provide FREE cardiac surgery to the underprivileged people of Fiji. Over the years the Foundation’s focus has expanded to include open heart surgery, pacemaker checks and implants, angiography, stenting, etc. Since 2006, treatments worth over NZ$10m have been performed with ZERO administrative costs. …
Ryan Hebbler

FUJIFIILM Sonosite employees are passionate about many things, helping people is at the top of the list. As is the case for Ryan Hebbler, our Director of Strategic Accounts, which means helping customers, colleagues, clinicians, and everyone else he deals with. He's passionate about ultrasound, and it shows. …
Carena Holmes

Carena Holmes, senior systems engineer sees the big picture and the details. She is always thinking about how to improve our systems and how teams can work more harmoniously. When asked about her favorite project, she replies with a secretive smile, but that just goes to show how interesting the work she's doing is. She's a creative thinker and a passionate advocate for her work. …
Keith Williams

Keith Williams, Executive Director of Program Management at FUJIFILM Sonosite, is celebrating his 25th anniversary with the company. When asked what keeps him coming back, Williams said, "It's the people. I get to work with some phenomenally talented and passionate people who are dedicated to making a difference in the world. And the products we make have a really important role to play in that." In addition to his work at FUJIFILM Sonosite, Williams is also a passionate music fan. He shared his top 5 songs of all time with, which you can enjoy below. …
From the CEO: Find Work that Matters

Find Work that Matters at FUJIFILM SonositeLife is finite, which makes time our most precious commodity.The COVID pandemic has taken this concept and dropped it right in the lap of millions of working people in this country. “Why am I spending the majority of my waking hours doing this work, and is that how I want to spend the time I have left on this planet?” Welcome to the Great Resignation. …
From the CEO: Core Values

Core Values: A focus on HOW we face challenges together
The last few years have challenged us all. They’ve made us think deeply about what matters in our lives. Many have been faced with choices they never dreamed they’d have to make, especially in the early days of the pandemic. Do I work and risk illness or possibly death, or expose my loved ones to the same? Do I stop working and possibly lose my home? If you own or run a business, do you remain open in an effort to keep your team employed or do you shut down to reduce the spread of disease? …
POCUS Goes Airborne for Helicopter Rescue
Emergency doctor Dr. Didier Moens is in charge of rescue missions in the Centre Médical Héliporté (CMH) of Bra sur Lienne, near Liège in Belgium. He believes access to point-of-care ultrasound (POCUS) on emergency helicopters is now essential for improving the care of critically ill patients: …
A Time to Reflect: Sonosite PX Celebrates a Year to Remember

Anniversaries are times to celebrate, but also times to reflect. At FUJIFILM Sonosite, we’re thrilled to recognize the one-year anniversary of the launch of Sonosite PX, our next generation point-of-care ultrasound system (POCUS) with the most advanced image clarity ever seen in a Sonosite system. …
Consider All Ultrasound Machine Costs of Ownership
When making a high investment in medical equipment it is important not only to compare the price and quality of each product, in these cases it begins to be necessary to analyze the total cost of ownership (TCO) during the useful life of the equipment, since it could happen that the indirect costs exceed the sale price, plus all the additional problems that can even lead to damage to the reputation of the hospital. …
Setting Up a Point-of-Care Ultrasound Program in the Neonatal Intensive Care Unit
Drawing on Dr. Jae Kim’s experience with implementing and leading POCUS programs in two U.S. children’s hospitals, this article provides a five-step roadmap to adoption of this imaging modality to improve the safety and quality of care in the NICU. Physician training, the most active uses, and opportunities for POCUS in neonatal medicine and case examples are discussed. The article also provides guidance on selecting a point-of-care ultrasound system for neonatology.
…
Solving revenue capture for POCUS – The importance of workflow management
HealthCare Business News sat down with Dr. John Hipskind, ultrasound GME director and ultrasound fellowship director at Kaweah Delta Medical Center, one of the first sites to use Sonosite Synchronicity™ workflow manager. Dr. Hipskind discusses the advantages of point-of-care ultrasound, from reducing phantom scans, to easing credentialing and QA processes, and improving revenue at his facility.
…
POCUS Profile: Dr. Pradeep Suryawanshi

Dr. Pradeep Suryawanshi, Professor & Head, Department of Neonatology at BVU Medical College, Pune, India has 15 years of experience in field of neonatology. He is the first person to commence point-of-care neonatal ultrasound and neonatal functional echocardiography courses in India. He recently shared his views about how the use of point-of-care ultrasound has made a significant impact in his routine clinical practice. …
Ready to Face the Pandemic: Sonosite PX Launches in a Moment of Crisis

This July, FUJIFILM Sonosite launched Sonosite PX, its newest ultrasound system, in the midst of the COVID-19 pandemic. Diku Mandavia, M.D., Chief Medical Officer of FUJIFILM Sonosite, sat down with sonographer and Sonosite’s Director of Marketing Development Jodi Miller to discuss how Sonosite’s newest ultrasound system can help frontline health care workers combat the pandemic and why Sonosite PX is uniquely suited for this global health crisis. …