The Mission
Since the formation of the Friends of Fiji Heart Foundation (FOFHF) in 2006, the Foundation has sent a mission to Fiji for each successive year to provide FREE cardiac surgery to the underprivileged people of Fiji. Over the years the Foundation’s focus has expanded to include open heart surgery, pacemaker checks and implants, angiography, stenting, etc. Since 2006, treatments worth over NZ$10m have been performed with ZERO administrative costs.
The mission involves sending a volunteer team of over 55 doctors, technicians and nurses who give up to 3 weeks of their time to provide the skills and expertise that are not present but needed so critically in Fiji.
In October of 2023, FUJIFILM Sonosite’s own Deb Stanley coordinated with the foundation to help enable a new mission. The New Zealand Territory Manager loaned her Sonosite PX ultrasound machine, known for its advanced image clarity, along with a variety of transducers including the T8-3.
The Numbers:
25 Patients had surgery and all survived. The calculated STS and RheSCORE (Mejia AV, Brazil 2018) mortality risk scores for these patients (2 to 3 valve heart operations) ranged between 12 to 26%, hence the survival of our cohort, thus far at 30 days; is EXCELLENT (100%). We continue to follow up patients with Dr Sukafa for 30 days, 1, 5, and 10 years after heart surgery
40 patients were initially screened by the pre-assessment team (Dr’s Merz, Chan and Musker at CWMH with outstanding support from local cardiologist Dr Sukafa), 7 refused surgery, 6 were deemed too sick and unlikely to survive surgery, 2 were offered surgery then did not arrive because of “child care issues (sic)” 3 patients from Lautoka, 7 from Labasa, 15 from Suva areas. Of the 25 17/25 (70%) were female. This is the highest cohort of females we have done since data collection was done. These are future mothers or mothers that have barely survived childbearing because of rheumatic heart disease and heart failure. 10 patients were less than 25 years of age (40%), this is the youngest cohort since data collection was done.
90% presented with NYHA 3 or more symptoms (very short of breath on minimal exertion) and 76% in AF (irregular heart rhythm that increases risk of stroke and reflects a heart that is decompensating. The patient is now very sick). 8 had very poor right ventricle function that made them very high risk surgical candidates.
45 valves were implanted in 25 patients
Of the 25 patients; 4 (16%) were 3 valves surgeries, 12 (48%) were double valve surgeries and 9 (36%) were single valves. 21 (84%) of patients had Left Atrial appendage ligation or tying off of the part of the heart which SIGNIFICANTLY reduces the risk of stroke long term in these patients. World medical litreature supports this small but significant additional procedure to our surgery and we hope that future missions and follow up sees this reduction in lifetime morbidity of rheumatic heart disease (RHD).
This mission reflects the sickest cohort of patients we have operated on yet. We suggest this is similar worldwide with COVID delays in admission for medical care, delay in diagnosis and recognition of the disease, reduced general health of the population and access to health care, recognition of RHD for the first time in periparturient (pregnant mothers) as a trial of life, and the inability of medical treatment to stall the effects of RHD. It is a devastating disease once diagnosed and unfortunately even with treatment some will require life-saving heart valve surgery.
Dr Sukafa, a local Cardiologist, has >160 patients in the Suva area alone, who will need heart surgery in the near future. She estimates about 30 died per year during the COVID period that the mission was not able to come to Fiji. This is likely a gross underestimate. One patient needed an urgent pacemaker post operative day 5, because our team is integrated; Cardiologist Dr Jonathan Tisch and his team safely implanted one to allow uninterrupted recovery. Two more patients were seen urgently.
The Mission Staff:
We continue to have excellent (nursing, medical, paramedical, perfusionists, CSSD, physiotherapists, technical and support) staff that make the mission a success. That the mission always flows with minimal impact on the patient’s surgery reflects the incredible effort, dedication and skills of the teams, but also the unmeasurable impact of team solidarity, experience, teamwork and focus on the patients. The tireless impact of Kirit, Aleem, Divend, Jasmeen, Jonathon (admin and logistics team) and so many other people is gratefully appreciated.
The deliberate inclusion of keen Fellows (senior registrars who are doing fellowship in Cardiothoracic anaesthesia or intensive care) means that succession and future leaders are a planned move.
One of the unsung, but incredible HEROES of the FOFHF mission to Suva was local Cardiologist: Dr Sukafa. If only I could tell you how hard she works for her patients, how much she cares for them, how much time and energy she gave to us as a visiting team; even though we likely doubled her workload. Yet she is humble and unassuming. Vinaka Vakalevu to her and her team.
A special thank you to the blood bank staff who worked tirelessly to provide us an excellent service for blood and product transfusion at all hours. Thank you to the CWMH superintendent Dr Luka, Dr Chima the radiology superintendent who allowed us to use the portable X-ray machine for ICU and the step down ward. It diagnosed 5 critical pneumothoraces that day (deflated lungs). We need good relationships with department leads and administration to smooth our way.
The Meat:
This was the leanest staffed mission we have run. Costs and post COVID challenges meant that an experienced, versatile team was important. Difficult logistics, spiraling costs of airfares and accommodation, financial and strategic contraction of medical companies and sponsors we have relied on before meant a tough mission in 2023.
We planned 6 operating days. 5 days for an intense 5 cases/two theatres caseload and a spare day for contingency. We started 3 days before the Mission theatre start with 40 patients preassessed.
This lead to long 12 to 14 hour days. We thought this would be the most cost efficient way given the severity of cases seen and planned. We apologize that some of the events organised for us by the sponsors and local FOFHM team we could not attend. “The person with their chest open in the theatre is the most important”
We made a start on a Monday which felt right and allowed for set up at CWMH. We planned a early start of 0630h for a “knife to skin” time of 0730h and ICU ward round at 0700h for the most sick day zero patients. We set an expectation of “respect, fair play, dress code, values and behaviour” on the Sunday on team brief to all team and team leaders. We set a clinical expectation of minimum twice a day ward rounds in ICU and step down wards with a Dr Nish Patel implemented consistent patient pathway for care that the nurses and patients could follow.
Handover to the medical wards was on day 5 or once warfarin levels were therapeutic. A unique patient code and front sheet and assessment A4 page was started at pre-assessment and designed to follow them through to discharge. This meant all medical data was legible, easy to follow and available. This we hope will make for easier follow up and data collection.
Very obvious in this mission was the impact of local media. Planned radio interviews, both in English and Hindi, TV interviews and press conferences provided much needed exposure of the mission to the public. Hopefully this makes future bridge building between the FOFHM and Government officials (Hon Antonio MOH) and sponsors easier . Building bridges with the new Fiji regime is critical for future success.
We are clinicians not media stars. But I appreciate that Dr Paul Musker, Jasmeen, Kirit and Aleem stood up and provided soundbites and critical explanations of the mission, of RHD prevention and connected the mission with stories of the patients who have had heart valve surgery. This must continue in the future. The exposure of the mission to the public, the dignitaries and sponsors is vital for its survival.
The Stories:
Of course our amazing patients have amazing stories. These are powerful and persuasive. These are Fiji’s woman, children and loved ones. They tell us in their journey about the disease of RHD, about hope and the effect of surgery on their lives:
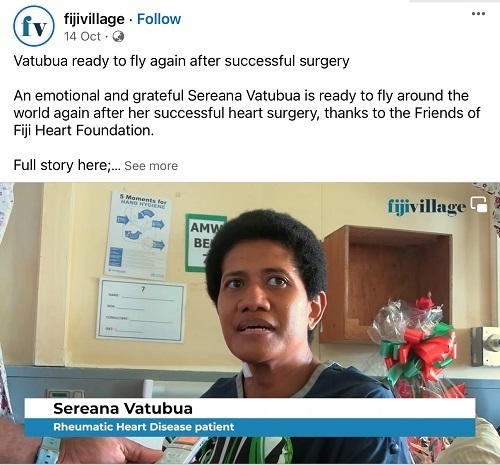
Surely the mission poster girl! Sereana, a flight attendant, is an ebullient, vivacious, well spoken woman who has the spirit of the women of Fiji. So sick she would likely lose her job without surgery, she not only was a great patient but also inspired the woman around her to take their medicines but also to live life. She was inspiring Rhadini; a 17 year old girl who had two valve surgery to be a flight attendant last I saw. A smile brighter than the Sun. Also in the room was Karita.
Sarei, a 21 year old woman wants to train to be a pilot. She had RHD in 2020 and thought she had COVID. She already was on Dr Sukafa’s books as a surgical candidate in 2020 but we were not able to go to Suva during COVID. She came on Wednesday because we had a space but due to a very sick long case in the theatre on Wednesday night I had to cancel her. According to her sister she was despondent. But we had no resources left. On Friday morning we had one valve left. And one last bed in ICU. We assessed Sarei and actually admitted her as she was so sick. Overnight on the ward she went into a fast heart rhythm and decompensated. Dr Musker admitted her to the ward and took 4 litres of water off her lungs. We assessed her at 0700h and decided surgery was now urgent and proceeded. Happily the valve, her heart and massive input from the team meant this morning (15 Oct) Sarei was extubated and sent to the ward. A very large smile not just on her face but also ours.
Amelia, a 35 year old crown prosecutor (married with two teenage children) has had rheumatic heart disease since 2011. She was so sick flying from Labasa that flight staff were reluctant to take her. She was so driven to have three valve heart surgery that by the time she was seen by the preassessment team she need to be admitted for heart failure. She had such a poor right and left heart that she needed a lot of heart drugs and time in ICU.
When extubated and woken up in the ICU on Saturday morning the first thing she did was write on a small piece of paper “thank you”.
Jesé who just turned 16 years of age and his schoolteacher mother Maria. Although largely asymptomatic, Jesé had severe three valve disease of his heart. His mother was so grateful her youngest son would have life saving three valve heart surgery by the team, and he recovered well.
You can learn more about the Friends of Fiji Heart Foundation in the links below: